The long-term impact of thrombotic thrombocytopenic purpura (TTP)
Patients can experience the effects of TTP long after their first episodes
The consequences of TTP can lead to many long-term complications and health risks. Approaching TTP with a long-term mindset can help ensure comprehensive care for your patients.1-3
Microthrombi may result in long-term neurocognitive decline in patients with TTP1
63% of patients with TTP have neurological signs and symptoms during their first event, including2-4
• Coma
• Focal neurological signs
• Personality changes
• Transient ischemic attack
• Seizures
• Stroke
In these patients, studies have shown4
Persistent neurological impairment during remission (49%)
• Disorientation
• Loss of concentration
• Dizziness
• Lack of balance
• Headache
• Diplopia
Significant impairment in memory domains
(direct, backward, and deferred memory) vs the general population
Higher prevalence of relapse in TTP
vs those without neurological symptoms (41% vs 8%)
Patients with TTP may have increased risk of stroke after recovery5
Stroke during the median observation follow-up period (3.08 years) after recovery from TTP occurred in 13.1% of patients, which is five-fold higher than the expected prevalence from an age- and sex-matched reference population.
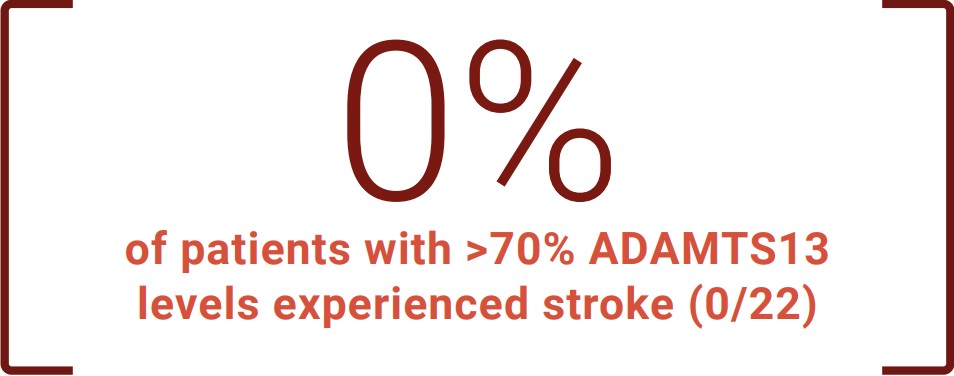
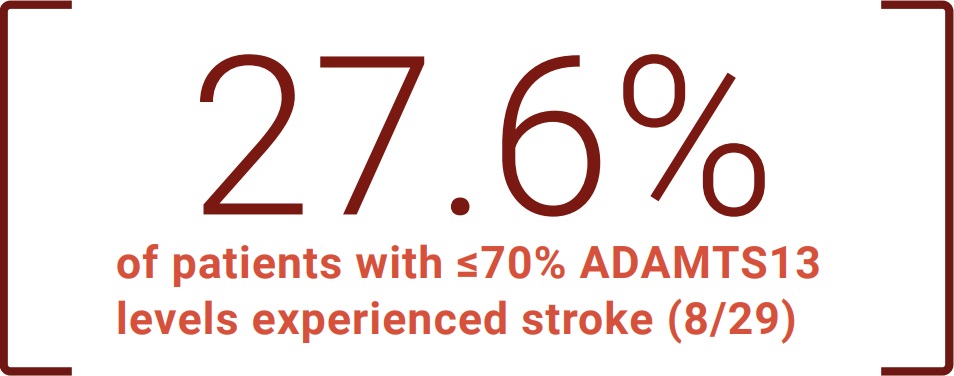
Stroke risk is common after recovery from TTP and is associated with ADAMTS13 levels
Low ADAMTS13 activity after recovery from an acute episode is associated with an increased risk of ischemic stroke during the follow-up period. (P=0.007)
Patients with TTP reported decreased quality of life1,4
TTP affects patients’ quality of life over the long term, owing to exacerbations, relapses, and sustained neurocognitive defects. Patients’ responses across health-related quality of life measures suggest that living with TTP is a considerable emotional burden.
Clinical anxiety and depression are serious risks for patients with TTP4
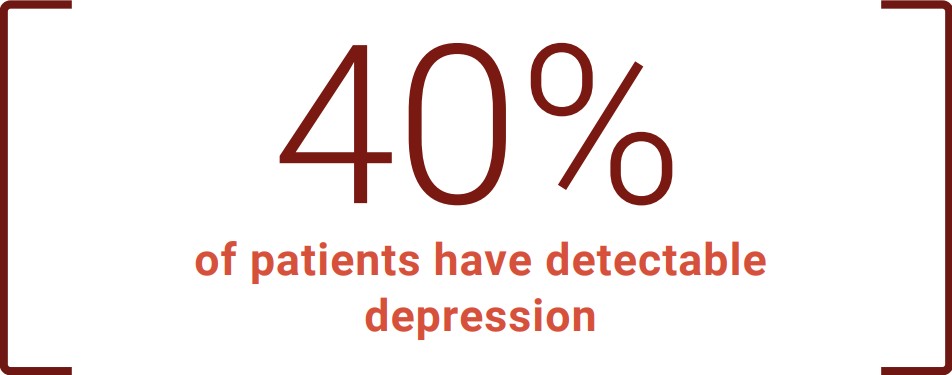
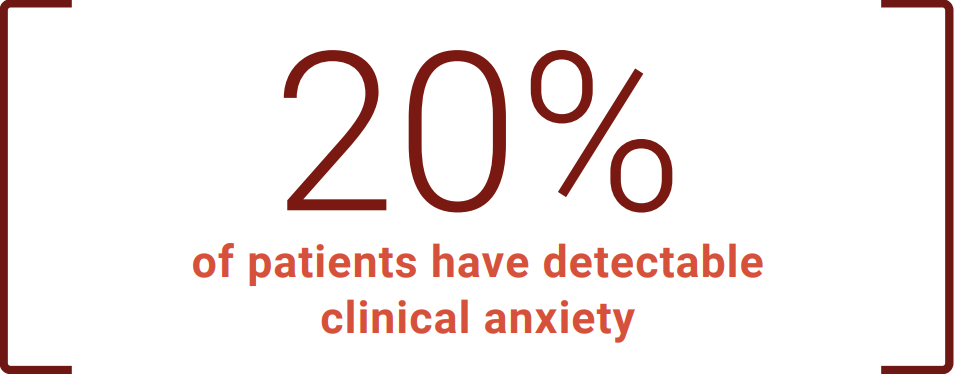
It's important to monitor the physical and mental health of your patients with TTP.1,4,5
Each person with TTP has a unique
experience.
There are a variety of resources to support
you and your patients.
ADAMTS13=a disintegrin and metalloproteinase with thrombospondin type 1 motif, 13.
References: 1. Zheng XL, Vesely SK, Cataland SR, et al. ISTH guidelines for the diagnosis of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020;18(10):2486-2495. doi:10.1111/jth.15006 2. Han B, Page EE, Stewart LM, et al. Depression and cognitive impairment following recovery from thrombotic thrombocytopenic purpura. Am J Hematol. 2015;90(8):709-714. doi:10.1002/ajh.24060 3. Deford CC, Reese JA, Schwartz LH, et al. Multiple major morbidities and increased mortality during long-term follow-up after recovery from thrombotic thrombocytopenic purpura. Blood. 2013;122(12):2023-2029. doi:10.1182/blood-2013-04-496752 4. Riva S, Mancini I, Maino A, et al. Long-term neuropsychological sequelae, emotional wellbeing and quality of life in patients with acquired thrombotic thrombocytopenic purpura. Haematologica. 2020;105(7):1957-1962. doi:10.3324/haematol.2019.226423 5. Upreti H, Kasmani J, Dane K, et al. Reduced ADAMTS13 activity during TTP remission is associated with stroke in TTP survivors. Blood. 2019;134(13):1037-1045. doi:10.1182/blood.2019001056

