Identifying thrombotic thrombocytopenic purpura (TTP) among thrombotic microangiopathies (TMAs)
TMAs require urgent management, but variable presentation can make them difficult to distinguish1,2
TMA is a pathologic term used to describe occlusive microvascular or macrovascular disease, often with intraluminal thrombus formation.3 Presentation of TMAs varies widely, including but not limited to stroke, neurologic complications, severe renal failure, flu-like symptoms, and simple fatigue.4,5
This leads to the involvement of several physician specialists at the outset of patient care in clinic and hospital settings. Both—the variability of TMAs and the involvement of many specialties—pose a challenge to prompt recognition and diagnosis of TTP.4,5
Your role is crucial to the diagnosis and speed of appropriate treatment for TMAs6
In most cases, patients present at the emergency department for a nonspecific somatic complaint, and thrombocytopenia is subsequently discovered. More rarely, the results of a CBC can reveal thrombocytopenia during an appointment in a non-hospital setting.6
It is critical to suspect TMA when you see7,8:
Thrombocytopenia
(defined as platelets <100 × 109/L)
Microangiopathic hemolytic anemia (MAHA)
characterized by the presence of
schistocytes in blood smear
Organ failure
of varying severity
Thrombocytopenia associated with MAHA should suggest a TMA syndrome, even in the absence of organ failure.9
-
Thrombocytopenia
-
Hemolytic anemia
-
Hyperbilirubinemia
-
Haptoglobin low, even undetectable
-
High LDH rate§
-
Most often normal
-
D-dimer rate may be moderately elevated
-
Thrombocytopenia
-
Hemolytic anemia
-
Hyperbilirubinemia
-
Haptoglobin low, even undetectable
-
High LDH rate§
-
Most often normal
-
D-dimer rate may be moderately elevated
|
Biological report sheet |
||
|
Blood count
|
|
|
|
|
|
|
|
Reticulocyte count |
High (>120 g/L)* |
|
|
Hemoglobin |
Low |
|
|
Schistocytes on blood smear |
Present† |
A hallmark of TTP, but absence |
|
Coombs test |
Negative‡ |
|
|
Hemolysis evaluation
|
|
|
|
|
|
|
|
|
While not diagnostic, elevated LDH |
|
|
Hemostasis assessment
|
|
|
|
|
|
|
Biological report sheet |
|
|
|
|
|
|
|
|
Reticulocyte count |
High (>120 g/L)* |
|
Hemoglobin |
Low |
|
Schistocytes on blood smear |
Present† A hallmark of TTP, but absence does not rule out a diagnosis |
|
Coombs test |
Negative‡ |
|
Hemolysis evaluation |
|
|
|
|
|
|
While not diagnostic, elevated LDH may predict organ damage |
|
Hemostasis assessment |
|
|
|
|
Understanding the types of TMAs can change how you treat the patient1,12
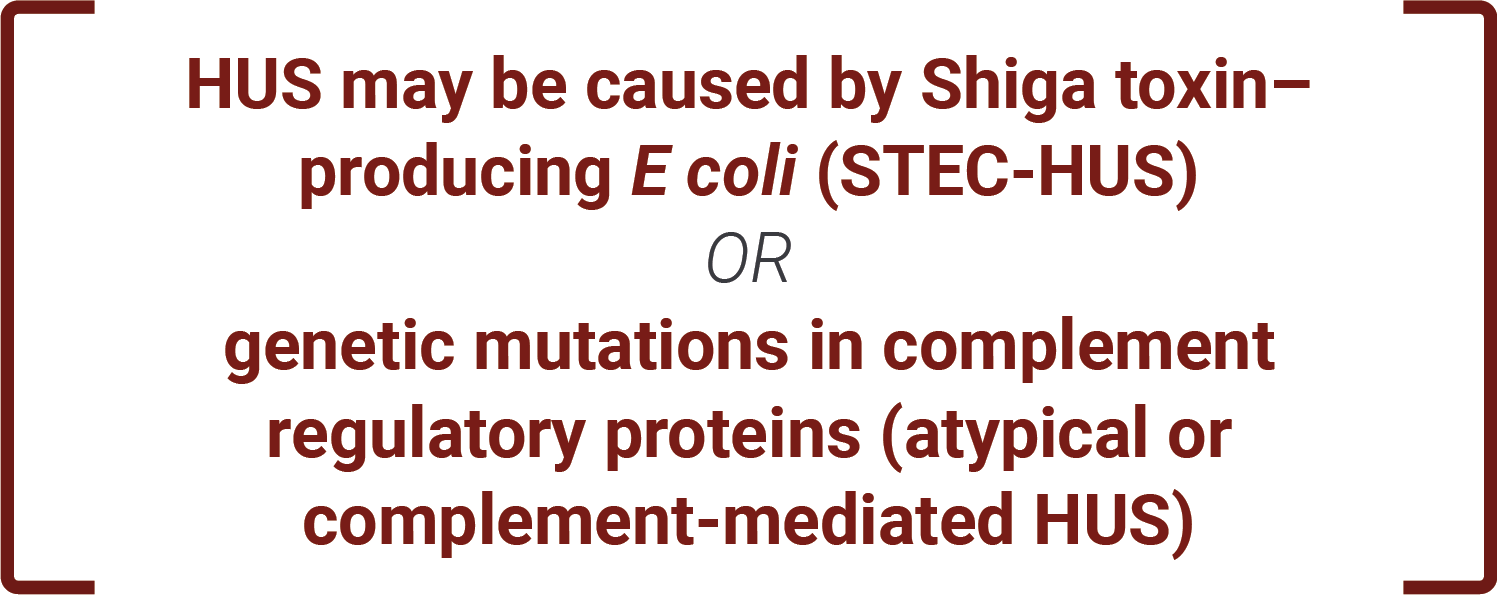
TMAs are classified into 2 types: primary and secondary. Primary TMAs have no clear underlying cause, while secondary TMAs may be caused by a number of clinical conditions. Recognizing the underlying cause, or lack thereof, can determine treatment course.1,12
-
TTP (acquired/immune-mediated and hereditary)
- Systemic lupus erythematosus
-
HUS (atypical/complement-mediated and Shiga toxin–producing E coli)
- Pregnancy-associated (eg, hemolysis, elevated liver enzymes, low platelet count [HELLP] syndrome)
- Hematopoietic progenitor cell transplantation
- Drug-induced
|
Primary TMAs |
Secondary TMAs |
|
|
|
|
|
|
|
|
|
|
|
The 2 primary TMAs—TTP and HUS—are often confused, but differentiating them is critical to determining appropriate treatment1,2
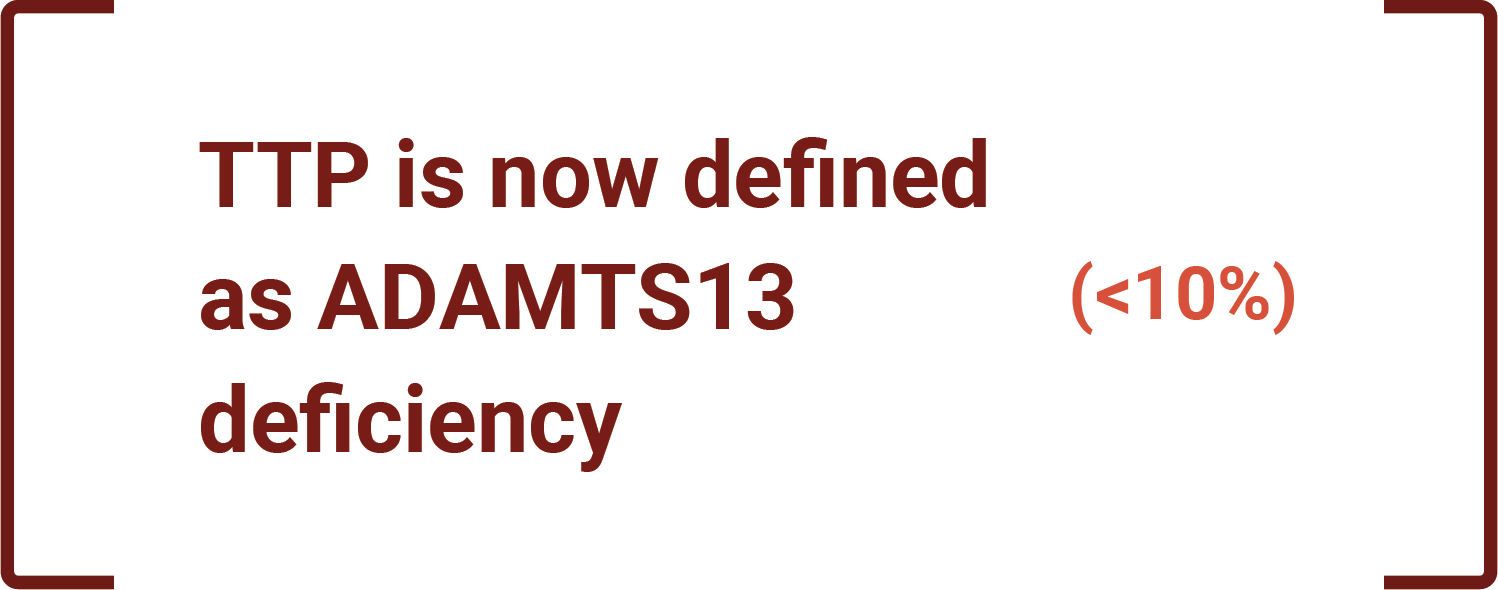
Historically, TTP and hemolytic uremic syndrome (HUS) were classified based on clinical findings: TTP for predominant neurologic involvement and HUS for the kidney-dominant diseases.1,13 With recent understanding of the molecular basis of TMAs, definitions have changed.1,7,8,11,13
VS
Differentiation of TTP from HUS can be confounded by kidney involvement in TTP. 25% of patients with TTP had kidney injury in the Oklahoma TTP Registry.5,14,15
Variable presentation of TMAs, potential confusion with HUS, and lack of diagnostic protocols can result in a missed or delayed diagnosis of aTTP2,16
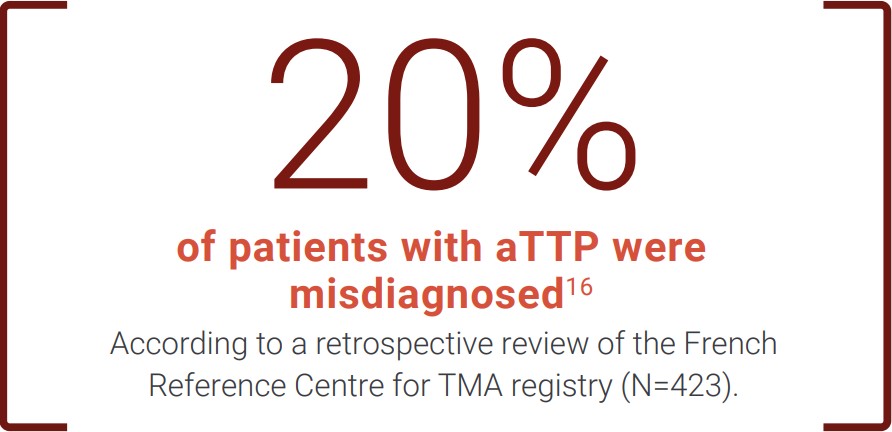
This number may be underestimated due to the study being unable to exclude the possibility that some misdiagnosed patients may have died before their TTP diagnosis was made.16
The consequences of delayed diagnosis and treatment of TTP can be devastating, including organ failure or even death.7,11,15-17
Rapid recognition of aTTP is critical to
outcomes.
Acute mortality and morbidity pose serious
risks in patients with aTTP.
aTTP=acquired thrombotic thrombocytopenic purpura; CBC=complete blood count; E coli=Escherichia coli; LDH=lactate dehydrogenase.
*Emphasizes the regenerative nature of anemia.
†Nonsystematic presence of schistocytes, possibly late onset, hence the importance of repeating this test several times to increase the sensitivity of the examination.16
‡Test may turn out to be slightly positive in an autoimmune environment.16
§Related to hemolysis and organ tissue damage.6
References: 1. Arnold DM, Patriquin CJ, Nazy I. Thrombotic microangiopathies: a general approach to diagnosis and management. CMAJ. 2017;189(4):E153-E159. doi:10.1503/cmaj.160142 2. Gallan AJ, Chang A. A new paradigm for renal thrombotic microangiopathy. Semin Diagn Pathol. 2020;37(3):121-126. doi:10.1053/j.semdp.2020.01.002 3. Scully M, Cataland S, Coppo P, et al. Consensus on the standardization of terminology in thrombotic thrombocytopenic purpura and related thrombotic microangiopathies. J Thromb Haemostasis. 2017;15(2):312-322. doi:10.1111/jth.13571 4. Bommer M, Wölfle-Guter M, Bohl S, Kuchenbauer F. The differential diagnosis and treatment of thrombotic microangiopathies. Dtsch Arztebl Int. 2018;115(19):327-334. doi:10.3238/arztebl.2018.0327 5. Coppo P, Veyradier A. Current management and therapeutical perspectives in thrombotic thrombocytopenic purpura. Presse Med. 2012;41(3 pt 2):e163-e176. doi:10.1016/ j.lpm.2011.10.024 6. Gardy O, Gay J, Pateron D, Coppo P. Les microangiopathies aux urgences. Presented at: Urgences 2014; June 4-6, 2014; Paris. Accessed February 18, 2022. https://www.sfmu.org/upload/70_formation/02_eformation/ 02_congres/Urgences/urgences2014/donnees/pdf/077.pdf 7. Joly BS, Coppo P, Veyradier A. Thrombotic thrombocytopenic purpura. Blood. 2017;129(21):2836-2846. doi:10.1182/blood-2016-10-709857 8. Zheng XL, Vesely SK, Cataland SR, et al. ISTH guidelines for the diagnosis of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020;18(10):2486-2495. doi:10.1111/jth.15006 9. Van der Linden T, Souweine B, Dupic L, Soufir L, Meyer P. Management of thrombocytopenia in the ICU (pregnancy excluded). Ann Intensive Care. 2012;2(1):42. doi:10.1186/2110-5820-2-42 10. Azoulay E, Bauer PR, Mariotte E, et al; Nine-i Investigators. Expert statement on the ICU management of patients with thrombotic thrombocytopenic purpura. Intensive Care Med. 2019;45(11):1518-1539. doi:10.1007/s00134-019-05736-5 11. Scully M, Hunt BJ, Benjamin S, et al; British Committee for Standards in Haematology. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158(3):323-335. doi:10.1111/j.1365-2141.2012.09167.x 12. Radhakrishnan J. Anticomplement therapies in “secondary thrombotic microangiopathies”: ready for prime time? Kidney Int. 2019;96(4):833-835. doi:10.1016/j.kint.2019.08.00f 13. Tsai H-M. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010;91(1):1-19. doi:10.1007/s12185-009-0476-1 14. George JN. The remarkable diversity of thrombotic thrombocytopenic purpura: a perspective. Blood Adv. 2018;2(12):1510-1516. doi:10.1182/bloodadvances.2018018432 15. Kremer Hovinga JA, Vesely SK, Terrell DR, Lämmle B, George JN. Survival and relapse in patients with thrombotic thrombocytopenic purpura. Blood. 2010;115(8):1500-1511. doi:10.1182/blood-2009-09-243790 16. Grall M, Azoulay E, Galicier L, et al. Thrombotic thrombocytopenic purpura misdiagnosed as autoimmune cytopenia: causes of diagnostic errors and consequence on outcome. Experience of the French Thrombotic Microangiopathies Reference Centre. Am J Hematol. 2017;92(4):381-387. doi:10.1002/ajh.24665 17. Sayani FA, Abrams CS. How I treat refractory thrombotic thrombocytopenic purpura. Blood. 2015;125(25):3860-3867. doi:10.1182/blood-2014-11-551580

