What is TTP?
Thrombotic thrombocytopenic purpura (TTP)—A rare, life-threatening medical emergency
TTP is a rare, life-threatening thrombotic microangiopathy (TMA). There are approximately 3 cases per million people.1,2
The name thrombotic thrombocytopenic purpura describes the 3 main characteristics of the disease.
Thrombotic: characterized by the formation of microthrombi (blood clots) within a blood vessel, which clog it and prevent blood circulation.
Thrombocytopenic: a lower-than-normal platelet count due to the consumption of platelets during microthrombi formation, which causes occlusion of microvasculature.
Purpura: spots of variable size on the skin or in the mucous membranes, due to small hemorrhages; they can be dark red and as small as a pinhead (petechiae) or purplish and 2 to 3 cm in diameter (ecchymosis).
Types of TTP
Acquired TTP3,4
-
aTTP, also known as immune-mediated thrombotic thrombocytopenic purpura (iTTP)
-
The most common form of TTP; approximately 95% of TTP cases are aTTP
-
Caused by autoantibody inhibition of ADAMTS13 activity
Hereditary TTP4,5
- Also known as congenital TTP, inherited TTP, familial TTP, or Upshaw–Schulman
syndrome - Very rare form of TTP; mainly detected in children
-
Caused by mutations in the ADAMTS13 gene
Primary aTTP vs secondary aTTP2,6,7
Primary aTTP
-
Primary aTTP refers to acquired autoimmune TTP for which there is no obvious underlying/precipitating cause/disease
-
Primary aTTP accounts for the majority of cases of TTP
Secondary aTTP
- Secondary aTTP refers to acquired autoimmune TTP for which a defined underlying disorder or trigger can be identified, including connective tissue disease (eg, systemic lupus erythematosus), HIV infection, cytomegalovirus infection, and/or a specific precipitating factor (eg, pregnancy or drugs)
-
Treatment of the underlying disorder and/or removal of the underlying precipitant
may be required, as well as standard TTP therapy
TTP causes systemic microthrombi and consequent thrombocytopenia, hemolytic anemia, and organ ischemia. These symptoms—coupled with TTP's rarity—can cause confusion with other TMAs, making TTP a challenge to diagnose.8-10
Signs and symptoms of aTTP include1,7-10
Petechiae, purpura, bruising
(skin)
Headache, confusion,
seizures, coma (neurological)
EKG abnormalities (cardiac)
Abdominal pain, diarrhea
(gastrointestinal)
Proteinuria/hematuria
(kidney)
Suspect aTTP?
The incidence of TTP is 2 to 6 per million individuals4
aTTP primarily affects young, healthy adults13,14
years of age on average
of people affected are women
higher aTTP incidence
in the Black population
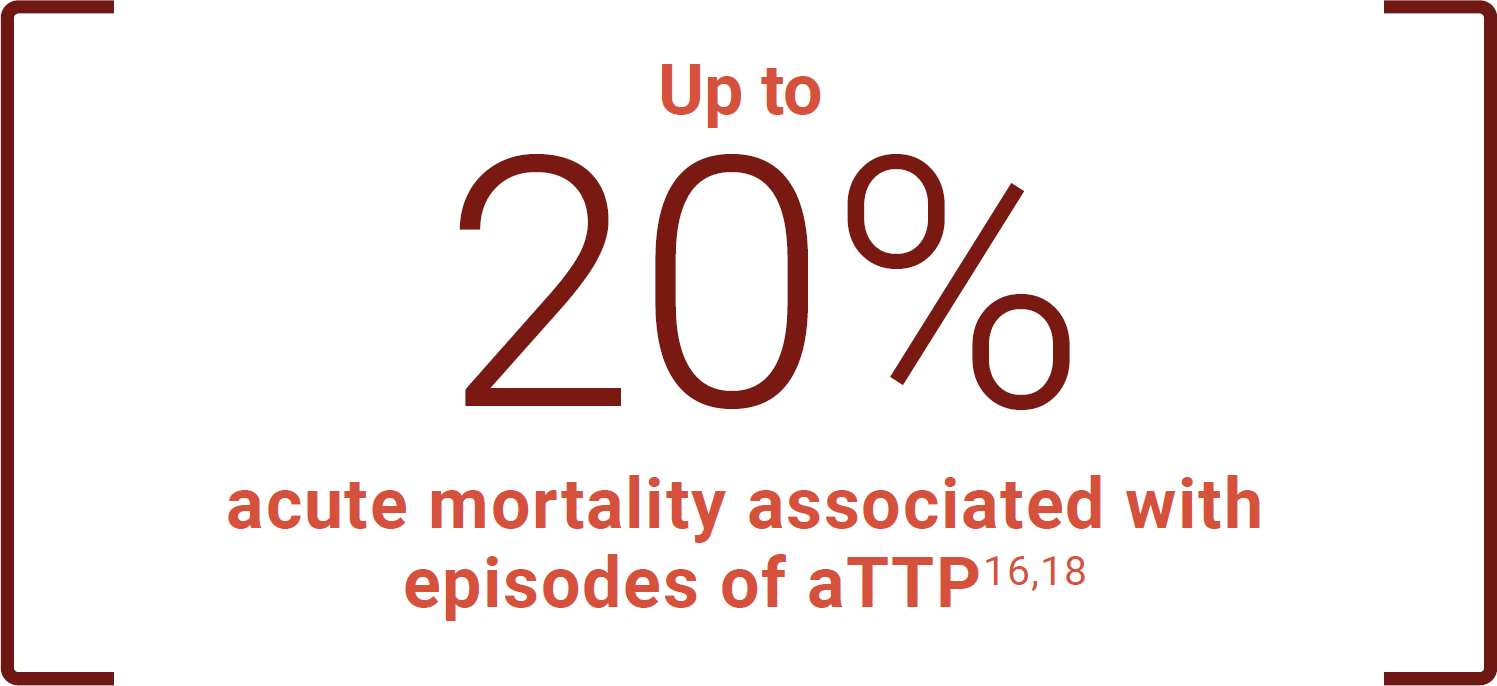
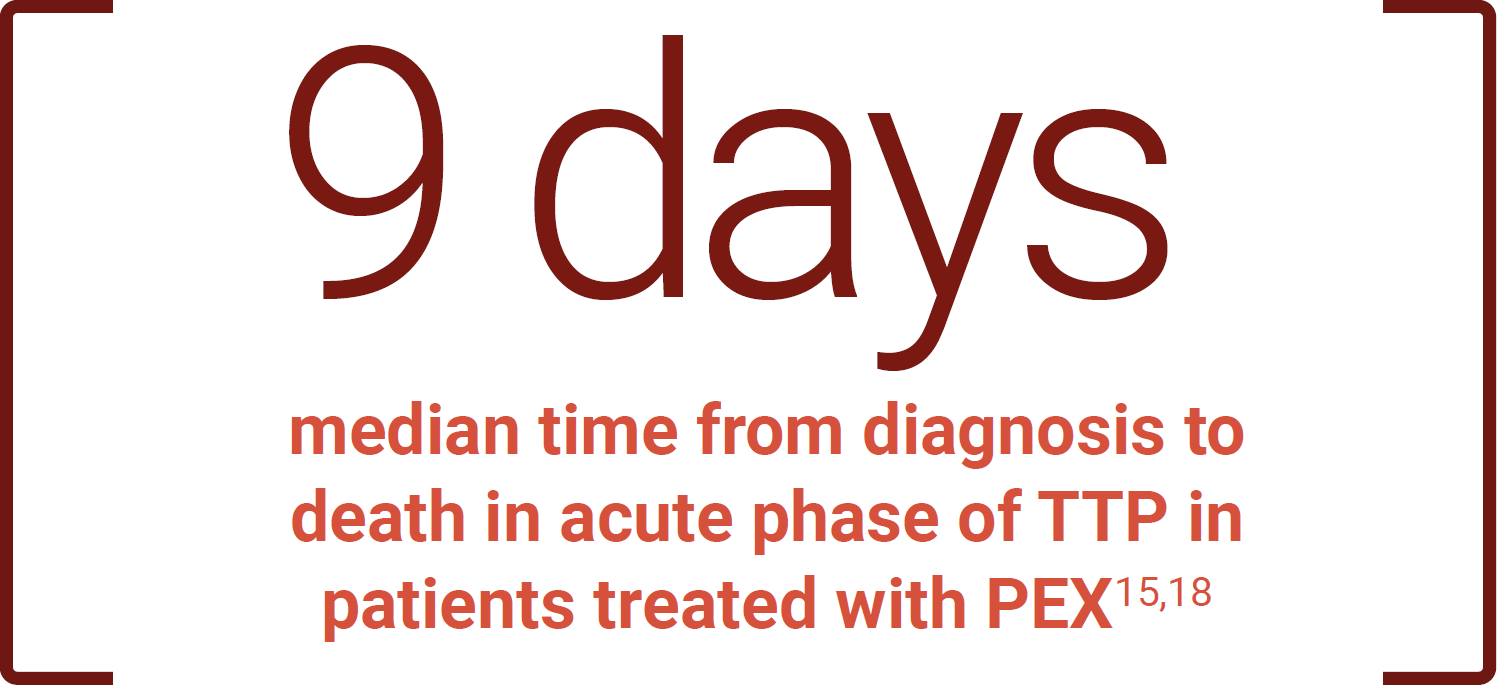
If left untreated, TTP is rapidly fatal8,15-17
acute mortality rate16,17
of TTP deaths occur within
24 hours of presentation8
Even with plasma exchange therapy (PEX), mortality risk persists5,16,18
Knowing the clinical science behind aTTP helps explain the severe effects of the disease.
Rapid recognition of aTTP is critical to outcomes.
ADAMTS13=a disintegrin and metalloproteinase with thrombospondin type 1 motif, 13; EKG=electrocardiogram.
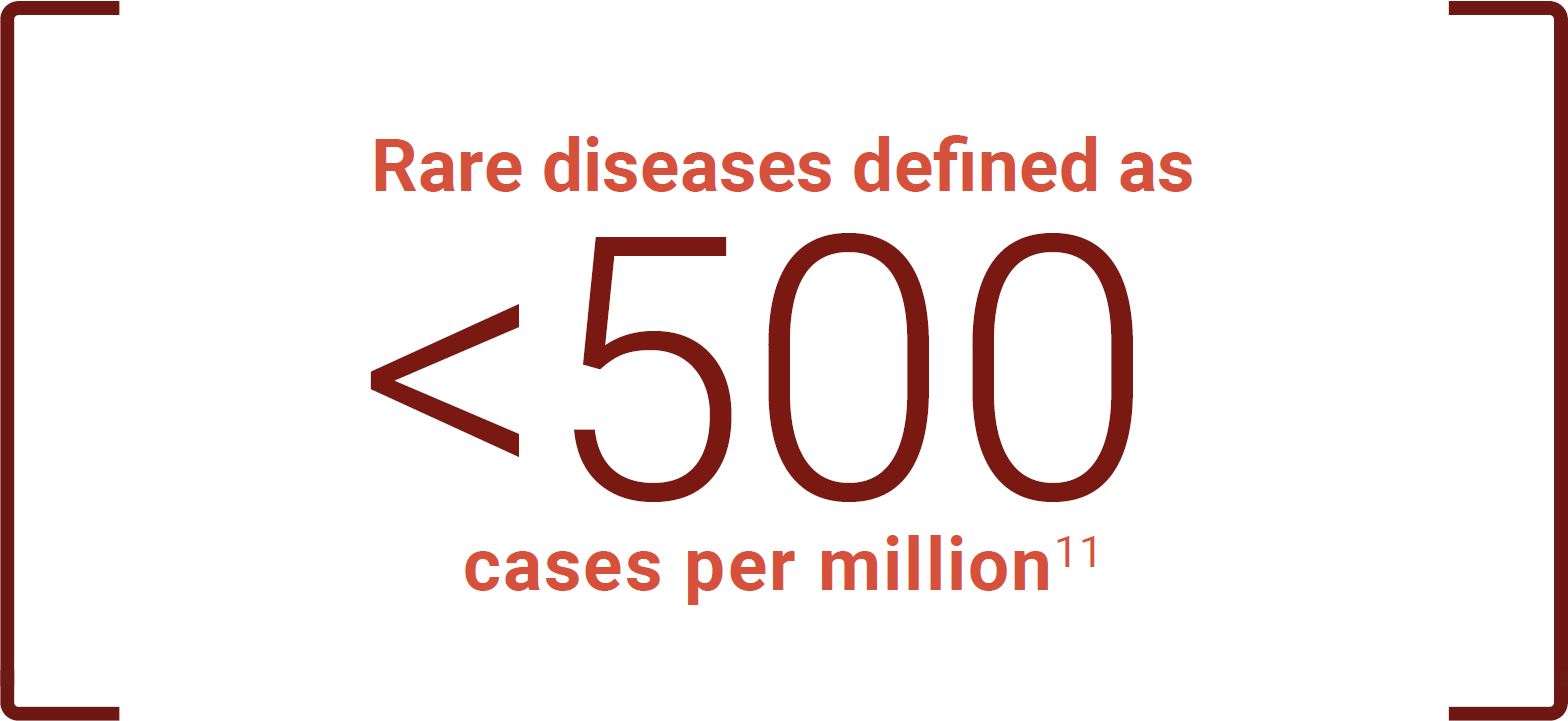
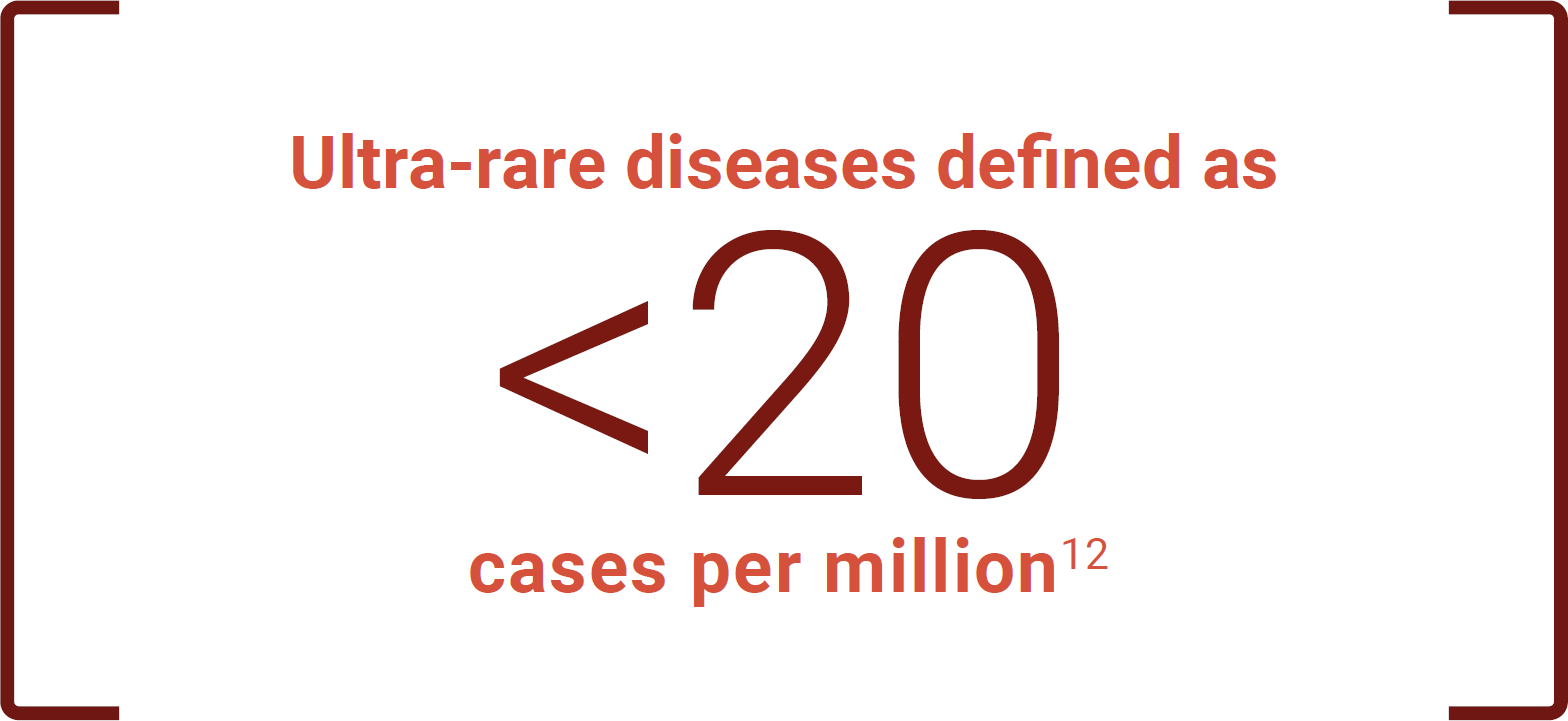
References: 1. Joly BS, Coppo P, Veyradier A. Thrombotic thrombocytopenic purpura. Blood. 2017;129(21):2836-2846. doi:10.1182/blood-2016-10-709857 2. Arnold DM, Patriquin CJ, Nazy I. Thrombotic microangiopathies: a general approach to diagnosis and management. CMAJ. 2017;189(4):E153-E159. doi:10.1503/cmaj.160142 3. Scully M, Cataland SR, Peyvandi F, et al. N Engl J Med. 2019;380(4):335-346. doi:10.1056/NEJMoa1806311 4. Zheng XL, Vesely SK, Cataland SR, et al. ISTH guidelines for the diagnosis of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020;18(10):2486-2495. doi:10.1111/jth.15006 5. National Institutes of Health. Congenital thrombotic thrombocytopenic purpura. Updated July 12, 2018. https://rarediseases.info.nih.gov/diseases/9430/congenital-thrombotic-thrombocytopenic-purpura 6. Sukumar S, Lämmle B, Cataland SR. Thrombotic thrombocytopenic purpura: pathophysiology, diagnosis, and management. J Clin Med. 2021;10(3):536. doi:10.3390/jcm10030536 7. Azoulay E, Bauer PR, Mariotte E, et al; Nine-i Investigators. Expert statement on the ICU management of patients with thrombotic thrombocytopenic purpura. Intensive Care Med. 2019;45(11):1518-1539. doi:10.1007/s00134-019-05736-5 8. Scully M, Hunt BJ, Benjamin S, et al; British Committee for Standards in Haematology. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158(3):323-335. doi:10.1111/j.1365-2141.2012.09167.x 9. Gallan AJ, Chang A. A new paradigm for renal thrombotic microangiopathy. Semin Diagn Pathol. 2020;37(3):121-126. doi:10.1053/j.semdp.2020.01.002 10. Tsai H-M. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010;91(1):1-19. doi:10.1007/s12185-009-0476-1 11. Kaplan W, Wirtz VJ, Mantel-Teeuwisse A, Stolk P, Duthey B, Laing R. Rare diseases. In: Priority Medicines for Europe and the World. 2013 Update. Chap 6.19. World Health Organization. https://www.who.int/medicines/areas/priority_medicines/MasterDocJune28_FINAL_Web.pdf?ua=1 12. Harari S, Humbert M. Ultra-rare disease: an European perspective. Eur Respir Rev. 2020;29(156):200195. doi:10.1183/16000617.0195-2020 13. Terrell DR, Williams LA, Vesely SK, Lämmle B, Hovinga JAK, George JN. The incidence of thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: all patients, idiopathic patients, and patients with severe ADAMTS-13 deficiency. J Thromb Haemost. 2005;3(7):1432-1436. doi:10.1111/j.1538-7836.2005.01436.x 14. Reese JA, Muthurajah DS, Kremer Hovinga JA, Vesely SK, Terrell DR, George JN. Children and adults with thrombotic thrombocytopenic purpura associated with severe, acquired Adamts13 deficiency: comparison of incidence, demographic and clinical features. Pediatr Blood Cancer. 2013;60(10):1676-1682. doi:10.1002/pbc.24612 15. Goel R, King KE, Takemoto CM, Ness PM, Tobian AAR. Prognostic risk-stratified score for predicting mortality in hospitalized patients with thrombotic thrombocytopenic purpura: nationally representative data from 2007 to 2012. Transfusion. 2016;56(6):1451-1458. doi:10.1111/trf.13586 16. Kremer Hovinga JA, Vesely SK, Terrell DR, Lämmle B, George JN. Survival and relapse in patients with thrombotic thrombocytopenic purpura. Blood. 2010;115(8):1500-1511. doi:10.1182/blood-2009-09-243790 17. Sayani FA, Abrams CS. How I treat refractory thrombotic thrombocytopenic purpura. Blood. 2015;125(25):3860-3867. doi:10.1182/blood-2014-11-551580 18. Peyvandi F, Scully M, Kremer Hovinga JA, et al. J Thromb Haemost. 2017;15(7):1448-1452. doi:10.1111/jth.13716

