The pathophysiology of thrombotic thrombocytopenic purpura (TTP)
TTP is characterized by potentially fatal systemic microthrombi1,2
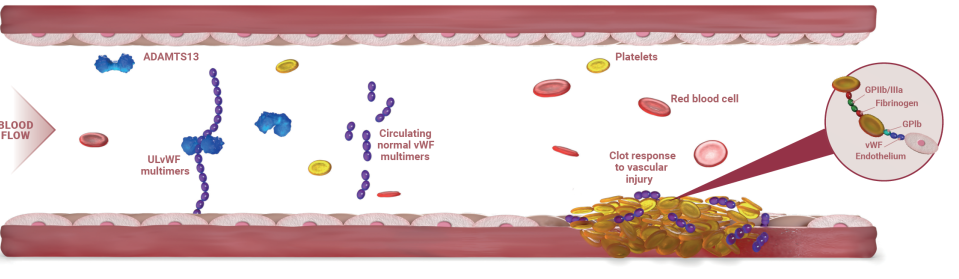
TTP is caused by severely decreased activity of the ADAMTS13 enzyme. ADAMTS13 is the protease that cleaves von Willebrand factor (vWF). In patients with acquired TTP (aTTP), this deficiency is immune mediated.1
Decreased ADAMTS13 activity leads to an accumulation of ultra-large von Willebrand factor (ULvWF) multimers, which spontaneously bind to platelets and induce aggregation. This results in dangerous microthrombi that drive severe thrombocytopenia, microangiopathic hemolytic anemia, and organ ischemia.2
TTP pathophysiology
An in-depth exploration of the causes of TTP and the severe consequences of the disease.
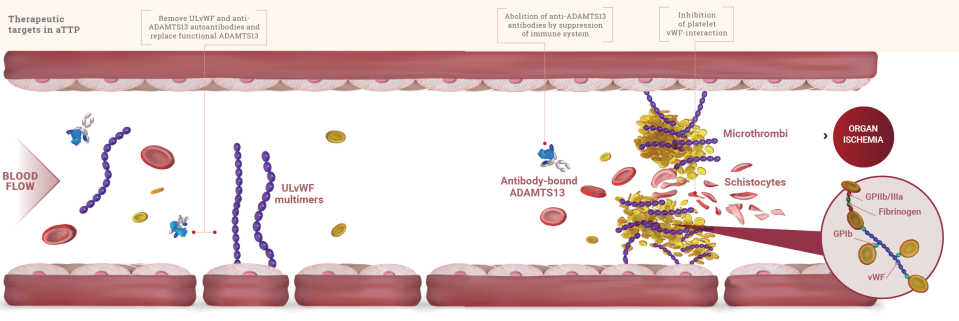
What is the pathophysiology of aTTP?
3 KEY MECHANISMS DRIVE THE PATHOPHYSIOLOGY OF aTTP2
Autoantibody formation
Autoantibodies to ADAMTS13 inhibit its activity or enhance clearance of the enzyme.
ADAMTS13 deficiency causes uncleaved ULvWF
ADAMTS13 (the enzyme responsible for cleaving vWF in the blood-clotting process) is deficient, leaving platelet-hyperadhesive ULvWF strands intact to circulate without being cleaved.

Microthrombi formation
ULvWF accumulates and spontaneously binds to platelets, forming microthrombi.
NORMAL PHYSIOLOGY2,3
THROMBOTIC THROMBOCYTOPENIC PURPURA2,3
Adapted from Joly B et al. Blood 2017 and Saad J & Schoenberger L 2018.
Formation of microthrombi causes2
Severe thrombocytopenia
(often platelets <30 × 109/L)
Microangiopathic hemolytic anemia (MAHA)
characterized by the presence of schistocytes in blood smear
Organ ischemia
(lesions can occur in any organ, but they most frequently affect the heart, brain, gastrointestinal tract, and kidney)

Understand the role of vWF

Learn about ADAMTS13
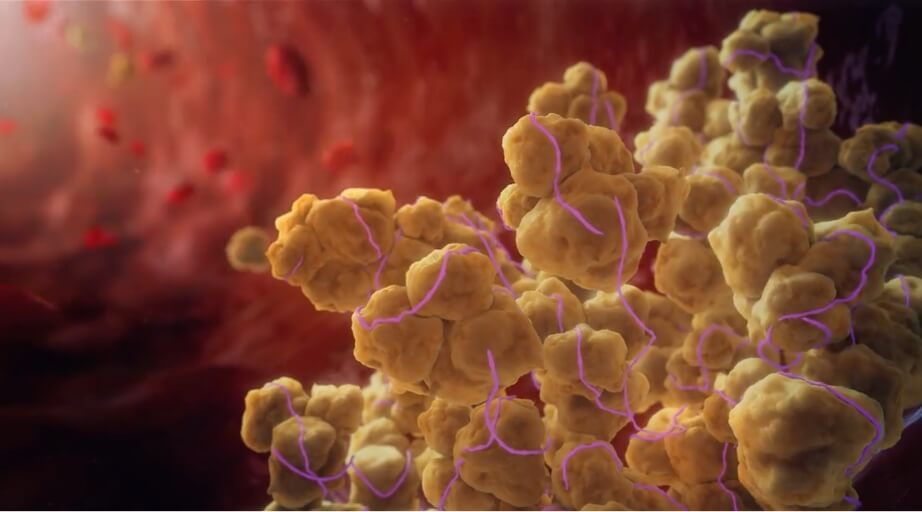
Platelet aggregation leads to microthrombi formation, which can have fatal consequences.1,2
The effects of TTP can be life-threatening.
Rapid recognition of TTP is critical to outcomes.
ADAMTS13=a disintegrin and metalloproteinase with thrombospondin type 1 motif, 13.
References: 1. Tsai H-M. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol. 2010;91(1):1-19. doi:10.1007/s12185-009-0476-1 2. Joly BS, Coppo P, Veyradier A. Thrombotic thrombocytopenic purpura. Blood. 2017;129(21):2836-2846. doi:10.1182/blood-2016-10-709857 3. Saad J, Asuka E, Schoenberger L. Physiology, platelet activation. Updated May 9, 2021. Accessed November 15, 2021. https://www.ncbi.nlm.nih.gov/books/NBK482478/

